Author: K. Michael Rowley, PhD
“Lumbar stabilization” is discussed both in clinical practice and in human movement and biomedical engineering research contexts, sometimes with different definitions or interpretations. Starting with “the problem” – it has long been understood that active contributions to lumbar spine stability are necessary to prevent buckling, given that buckling occurs in cadaveric models at as low as 88 N of vertical compression.(1) But this “stability” has diverse meanings for different audiences. Generally, stability refers to a system’s tendency to return to its unperturbed state after a perturbation.(2) For a clinician, this is assessed visually by how a person looks when they perform a task. The clinician examines aspects of motion like variability of the movement, speed of the movement, and the presence of any out-of-plane or compensatory motions to determine if the lumbar spine is “stable”. There are many active mechanisms that contribute to lumbar spine stability in a clinical sense, and through research we continue to learn about more. You may already be familiar with some mechanisms including contraction of deep paraspinal muscles, regulating intra-abdominal pressure, and functional bracing. Here, we will explore another contributor to stability – balancing forces in the connective tissue and fascia around the lumbar spine region.
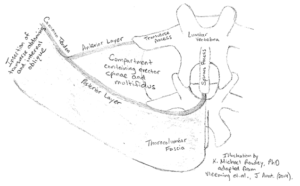
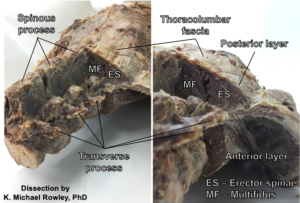
Thoracolumbar fascia has a posterior layer which arises from the midline of the lumbar spine over the spinous processes and wraps around the posterior side of the paraspinal compartment as well as an anterior or middle layer which arises from transverse processes and covers the anterior side of the paraspinal compartment meeting the posterior layer laterally where they serve as attachments for the common tendon of the transversus abdominis and the internal oblique muscles.(3) Two research groups have investigated this region of fascia by dissecting this tissue from a cadaver. Using quite a creative design, researchers examined the influence of intra-compartmental pressure by replacing the erector spinae and multifidus with a balloon and adding air to it, simulating contraction of the paraspinals. Alone, this did not stabilize the lumbar spine. Next, they simulated deep abdominal contraction by pulling on the common tendon portion of the fascia anteriolaterally, and this also did not increase lumbar spine stability. When both of these were done simultaneously, however, Vleeming et. al. reported that a “self-bracing” of the spinewas achieved.(3) Richardson et. al. found some in vivo evidence supporting this idea by measuring increased sacroiliac joint stiffness (measured using ultrasound Doppler) with contraction of the abdominals when lying prone.(4) Therefore, a balance of the forces – some forces pulling anterior from the abdominals and some posterior from paraspinal contraction causing an ‘inflation’ of the paraspinal compartment – is necessary to take advantage of the stabilizing ability of the thoracolumbar fascia.
Another research group, Tesh et. al., wanted to compare this effect to the better-known stabilization mechanism of intra-abdominal pressure. In addition to the methods described above, Tesh et. al. simulated intra-abdominal pressure by inflating balloons in an intact cadaveric abdominal cavity.(5) It turns out that intra-compartmental and intra-abdominal pressure increases had similar effects on lumbar spine stiffness in the sagittal plane, but the effects of balanced forces on the thoracolumbar fascia were more local while the effects of intra-abdominal pressure were more spread out along the length of the lumbar spine.(5) Intra-abdominal pressure also increased stiffness in the frontal plane, which the thoracolumbar fascia did not.(5)
Clearly, contributions to lumbar spine stability are complex and multi-factorial. This may be why McGill suggests “functional bracing” as the goal for effective and safe trunk control, where mechanisms utilized to stabilize the trunk must be tailored to the specific task demands and goals.(6) As we continue to learn about how the human body actively stabilizes the lumbar spine, we will continue to be able to leverage these mechanisms in the rehabilitation of debilitating conditions like low back pain.
About the Author:
 Michael Rowley is a recent graduate of the University of Southern California’s Division of Biokinesiology and Physical Therapy where he earned his PhD in Biokinesiology studying under the advisement of Dr. Kornelia Kulig. Michael’s dissertation research utilized a novel Balance-Dexterity Task(7) to investigate trunk control in persons with and without recurrent low back pain. He has also been involved in collaborative research projects investigating foot and ankle function and novel interventions for flexor hallucis longus tendinopathy in dancers. Michael currently teaches Musculoskeletal and Analytical Anatomy courses in the USC Physical Therapy program as an Assistant Professor of Clinical Physical Therapy.
Michael Rowley is a recent graduate of the University of Southern California’s Division of Biokinesiology and Physical Therapy where he earned his PhD in Biokinesiology studying under the advisement of Dr. Kornelia Kulig. Michael’s dissertation research utilized a novel Balance-Dexterity Task(7) to investigate trunk control in persons with and without recurrent low back pain. He has also been involved in collaborative research projects investigating foot and ankle function and novel interventions for flexor hallucis longus tendinopathy in dancers. Michael currently teaches Musculoskeletal and Analytical Anatomy courses in the USC Physical Therapy program as an Assistant Professor of Clinical Physical Therapy.
References:
- Crisco JJ, Panjabi MM, Yamamoto I, Oxland TR. Euler stability of the human ligamentous lumbar spine. Part II: Experiment. Clin Biomech. 1992;7(1):27-32. doi:10.1016/0268-0033(92)90004-N.
- Reeves NP, Narendra KS, Cholewicki J. Spine stability: the six blind men and the elephant. Clin Biomech (Bristol, Avon). 2007;22(3):266-274. doi:10.1016/j.clinbiomech.2006.11.011.
- Vleeming A, Schuenke MD, Danneels L, Willard FH. The functional coupling of the deep abdominal and paraspinal muscles: The effects of simulated paraspinal muscle contraction on force transfer to the middle and posterior layer of the thoracolumbar fascia. J Anat. 2014:447-462. doi:10.1111/joa.12227.
- Richardson CA, Snijders CJ, Hides JA, Damen L, Pas MS, Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine (Phila Pa 1976). 2002;27(4):399-405. doi:10.1097/00007632-200202150-00015.
- Tesh KM, Dunn JS, Evans JH. The abdominal muscles and vertebral stability. Spine (Phila Pa 1976). 1987;12(5):501-08.
- McGill SM. Low back stability: From formal description to issues for performance and rehabilitation. Exerc Sport Sci Rev. 2001;29(1):26-31. doi:10.1097/00003677-200101000-00006.
- Rowley KM, Gordon J, Kulig K. Characterizing the balance-dexterity task as a concurrent bipedal task to investigate trunk control during dynamic balance. J Biomech. 2018. doi:10.1016/j.jbiomech.2018.07.014.